 TB is classically thought of as a pulmonary disease–and in general, this is true, as pulmonary TB is by far the most common (and often very severe) manifestation of infection by Mycobacterium tuberculosis. However, the most common NON-pulmonary manifestation of TB worldwide is infection of the genitourinary tract, accounting for about 27% of non-pulmonary TB in most series according to this 2001 JASN review.
TB is classically thought of as a pulmonary disease–and in general, this is true, as pulmonary TB is by far the most common (and often very severe) manifestation of infection by Mycobacterium tuberculosis. However, the most common NON-pulmonary manifestation of TB worldwide is infection of the genitourinary tract, accounting for about 27% of non-pulmonary TB in most series according to this 2001 JASN review.
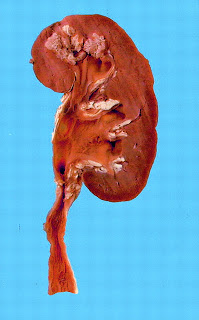
The name “renal tuberculosis” is a little misleading, since TB infection can actually cause renal problems by a variety of different mechanisms. Renal involvement may occur as part of a constellation of symptoms with miliary TB, in which there is mycobacterial “bacteremia/septicemia”. The preferred site for mycobacteria in the kidney is the renal medulla, where caseating granuloma can lead to necrosis and tissue destruction, occasionally resulting in papillary necrosis. Large caseating necrotic areas can lead to a clinical picture very similar to pyelonephritis. Alternatively, infection in the lower urinary tract can lead to anatomic abnormalities, such as ureteric strictures, which over time can progress to frank obstruction and even ESRD. In addition to these more “mechanical” explanations for renal failure, there have been several reports that chronic tuberculosis infection is a potential cause for tubulointerstitial nephritis. In India, where TB is very common, AA amyloidosis secondary to the chronic inflammatory state induced by TB infection is a well-recognized cause of kidney damage.
Genitourinary TB may be diagnosed by culture or PCR of the organism from the urine (or sputum, if there is pulmonary involvement). Detecting acid-fast bacilli from the urine is another possibility though apparently this is less specific than culture or PCR as there are some environmental mycobacterial species which may colonize the lower urinary tract. Renal TB may be suspected if the patient has signs and symptoms of a urinary tract infection with a workup that demonstrates pyuria but a negative urine culture. Obviously, travel/occupational history plays an important role in identifying individuals who are at higher risk for TB. Another clue to the diagnosis of renal TB is hypercalcemia: instead of being mildly hypocalcemic like most advanced CKD patients, patients with TB infection may have high levels of 1,25(OH) vitamin D as a result of granulomas having the ability to synthesize active vitamin D, similar to the situation in sarcoidosis. In the U.S., a very low percentage of patients (.004%) list TB as a cause for their ESRD, but in some European countries (e.g. Greece) the percentage is as high as 5%, and likely much much higher than this in many African countries. It is important to recognize in that TB is very much a treatable disease (and therefore a preventable cause of CKD/ESRD).